


Platelet-rich plasma (PRP) and Platelet-rich fibrin (PRF) are becoming a valuable adjunct to promote healing in many procedures in dental and oral surgery.
PRP & PRF are commonly applied in many dental and oral surgical procedures such as periodontal surgery, implant surgery and tooth extractions.


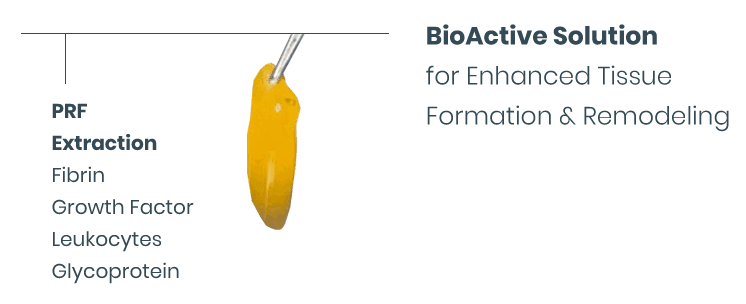
Tropocells® Pure PRF (Platelet Rich Fibrin) is an autologous
polymerised fibrin scaffold consists of large quantity of
platelet cytokines, growth factors and chemokines.
Tropocells® Pure PRF creates a fibrin scaffold with which the growth factors and other bioactive materials interact to stimulate the healing process. The Tropocells® pure PRF is generated following platelets activation which are trapped in this matrix. PRF is used to promote wound healing, bone regeneration, graft stabilization, wound sealing and haemostasis.
Tropocells® pure PRF advantages over the common PRF methods include, among others, ease of preparation/application, minimal expenses and lack of biochemical modification (no bovine, thrombin or anticoagulant is required).
A simple and fast preparation method.
Tropocells® pure PRF is prepared by taking either a 12ml or 23ml blood from the patient, then separating platelets from Red Blood Cells and Granulocytes via centrifugation. The clot that is formed is placed on the surface of a wound or is packed into a cavity or sinus. Platelets will be formed in a PRF matrix. As the clot dissolves, growth factors and other bioactive components in this milieu of autologous material are released. The Tropocells® PRF is generated without the addition of activating substances.
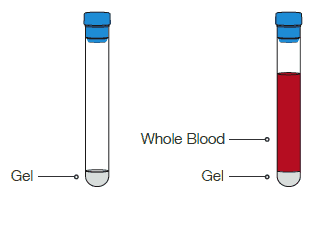
Collect blood directly into Tropocells® Pure PRF vacuum tube containing separation gel
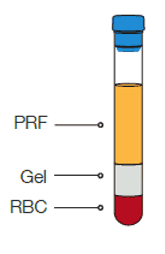
Immediately Centrifuge
for 15 min at 1500g

Gel sperarates plateles from RBC and
granulocytes. platelets are formed in
a PRF matrix
Enter a spatule to collect the PRF matrix
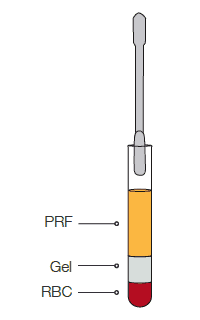
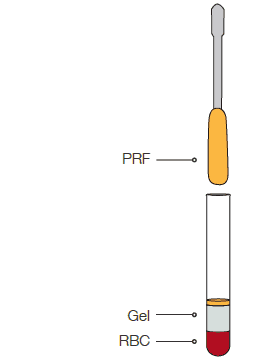
PRF is ready to use
The PRF Process
Tropocells®
pure PRF
Membrane Preparation
Why using PRP/PRF in dentistry?
Lower Infection Risk – PRP is smeared thickly on the wound after a dental procedure and actually seals the wound away from infectious agents, lowering the risk of problems.
Accelerated Healing – The saturation of the wound with PRP/PRF helps increase tissue synthesis due to its growth factors, and this in turn results in faster tissue regeneration. Speedier healing decreases the risk of later infections, complications and discomfort.
When PRP/PRF is used in conjunction with graft it improves trabecular bone density. Patients that received a mixture of PRP/PRF along with autologous bone, showed better epithelization and compact mature bone with well-organized trabeculae compared to the control group.
PRP/PRF jump starts osteogenesis by releasing growth factors at the local site and early consolidation of graft. This allows placement of implant into the grafted site at an early time.
BRON treatment (bisphosphonate-related osteonecrosis of the jaw) – bisphosphonates are widely used however they limit the healing ability by repressing growth factors.
Main applications:
- Bone defects
- Bone graft
- Sinus lift
